Bone health and weight management -
A person can absorb vitamin D through moderate sun exposure. Without sufficient vitamin D, a person has a higher risk of developing bone disease, such as osteoporosis or osteopenia. A moderate weight is essential for bone density.
People with underweight have a higher risk of developing bone disease. Overweight and obesity put additional stress on the bones.
Doctors recommend people avoid rapid weight loss and cycling between gaining and losing weight. As a person loses weight, they can lose bone density, but gaining back the weight will not restore bone density.
This reduction in density can lead to weaker bones. Super low calorie diets can lead to health problems, including bone density loss. Before restricting calories, discuss calorie needs with a qualified healthcare professional, such as a primary care doctor or registered dietitian, to determine a safe target number of calories to consume.
Protein plays an essential role in bone health and density. A cross-sectional study examined bone mass and dietary protein intake in 1, older adults. Researchers associated higher bone mass density with higher intakes of total and animal protein.
However, they associated lower bone mass density with plant protein intake. Researchers call for further studies, particularly into how a plant-based diet may affect bone health and density. Research suggests that omega-3 fatty acids play a role in maintaining bone density and overall bone health.
Like calcium, magnesium and zinc are minerals that support bone health and density. Magnesium helps activate vitamin D so it can promote calcium absorption.
Zinc exists in the bones. It promotes bone growth and helps prevent the bones from breaking down. Many people associate smoking with lung cancer and breathing issues, but smoking can also increase the risk of conditions such as osteoporosis and bone fractures. To support healthy bone density, a person can avoid or quit smoking , especially during their teens and young adulthood.
However, long-term heavy drinking can lead to poor calcium absorption, a decrease in bone density, and the development of osteoporosis later in life. Moderate alcohol consumption is considered two drinks or fewer per day for males and one drink or fewer per day for females. Although the best time to influence peak bone mass and build bone density is from childhood to early adulthood, people can take steps at every age to improve bone health and reduce bone density loss.
Strength training exercises can increase bone density in specific parts of the body in the short and medium term. However, people need to continue exercising regularly to maintain bone health in the long term. Bone mass peaks in young adults, usually between 25 and 30 years old.
After 40 years old, people start to lose bone mass. However, they can reduce this loss by exercising regularly and eating a balanced, nutrient-dense diet. Dietary intake of calcium and vitamin D is vital for bone health. Foods that contain these nutrients include:. To support healthy bone density, it is important to consume plenty of calcium, vitamin D, protein, and vegetables.
It is also important to avoid smoking and heavy alcohol use. Taking these steps can help support bone density throughout adulthood. Read this article in Spanish. A Z-score compares a person's bone density with the average bone density of those of the same age, sex, and body size.
A low score can indicate…. Bone density tests help a doctor see how strong a person's bones are. Learn more, including what happens during a bone density test, in this article. Femoral neck osteoporosis refers to a low bone density at the top of the thigh bone, and it puts people at a high risk of fractures.
Learn more. My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us.
Medical News Today. Health Conditions Health Products Discover Tools Connect. Medically reviewed by Stella Bard, MD — By Jenna Fletcher — Updated on January 4, Strength training Vegetables Calcium Vitamins Moderate weight Eat enough calories Protein Omega-3 fatty acids Magnesium and zinc Not smoking Avoid heavy alcohol use Is it too late?
FAQ Summary Low bone density can increase the risk of fracture. Weightlifting and strength training. Eat more vegetables. Consume calcium throughout the day.
Eat foods rich in vitamins D and K. Maintain a moderate weight. However, the data revealed the importance of including a control group with no weight loss, given that aging itself is associated with bone deterioration. Haywood et al. Total body BMD was assessed by DXA as the sole skeletal health outcome at baseline and at 12 weeks follow-up.
The exercise plus very low-calorie diet group experienced greatest weight loss, accompanied by a small, but significant, reduction in total body BMD; no significant changes were observed in the other study arms [ 41 ]. Additional evidence on the effects of exercise added to weight loss were obtained from 2 further RCTs [ 36, 42 ].
In a first small cohort, the effects of a lifestyle intervention consisting of caloric restriction, calcium and vitamin D supplementation, and a combined aerobic and resistance training program were compared to no treatment.
The reductions in hip BMD were correlated with elevations in CTX ~fold and osteocalcin ~fold , indicating that the bone loss was mediated by an uncoupling of bone formation from resorption, favoring the latter. BMD was maintained at the lumbar spine, which was suggested to be a bone-protective effect of exercise [ 42 ].
In a subsequent study by the same group, obese and frail older adults were randomized to no treatment, caloric restriction, exercise without weight loss, or caloric restriction combined with exercise [ 36 ]. The group that was randomized to caloric restriction combined with exercise experienced less hip bone loss than those who followed caloric restriction alone.
Unlike the group subjected to caloric restriction, the combined exercise and caloric restriction group did not experience changes in bone turnover markers or bone structure cross-sectional area, cortical thickness, and volumetric BMD at the 1-year follow-up, although trabecular microarchitecture was not assessed [ 31, 37 ].
These results suggest that a combination of resistance and aerobic training added to a weight loss program can lessen the bone loss induced by weight reduction. More recent studies have focused on the exercise type that would be most beneficial for weight loss in obese older individuals [ 39, 44, 45 ].
In a 6-month RCT, Villareal et al. Beaver et al. Volumetric BMD and cortical thickness estimates at the hip and femoral neck assessed by CT scans were significantly declined in all groups, with the most pronounced changes seen in the diet-induced weight loss group [ 39 ].
In a pooled analysis of the 3 treatment groups, bone strength estimated with subject-specific finite-element models based on CT-derived parameters was reduced by 6. Although this sub-analysis was not powered to detect between-group differences, finite-element models can be used to provide better predictions of bone strength and fracture risk in future weight loss interventions.
Taken together, these findings suggest that resistance training exerts bone-sparing effects in weight loss interventions which, however, may not always be captured by BMD assessed by DXA.
The discrepant results between the studies may be explained by differences in exercise regimens and the baseline characteristics of the study populations. Frail and obese individuals are possibly more responsive to the effects of exercise training. In a month follow-up of a 1-year weight loss intervention [ 36 ], Waters et al.
Similarly, Beavers et al. Both studies support unfavorable changes in skeletal health due to long-term weight loss. These studies were subject to reporting bias because they were based on subsets of the initial groups and did not include individuals with no weight loss. Nevertheless, they underpin the need for follow-up studies to evaluate weight management approaches in the elderly and characterize skeletal health outcomes associated with sustained weight loss or multiple weight loss attempts.
We investigated the available evidence on the mechanistic links between weight loss and bone loss in obese older individuals or relevant aged animal models.
We also discuss speculative contributors to bone loss during weight loss which, however, have been poorly investigated in obese elderly under weight loss and require further elucidation.
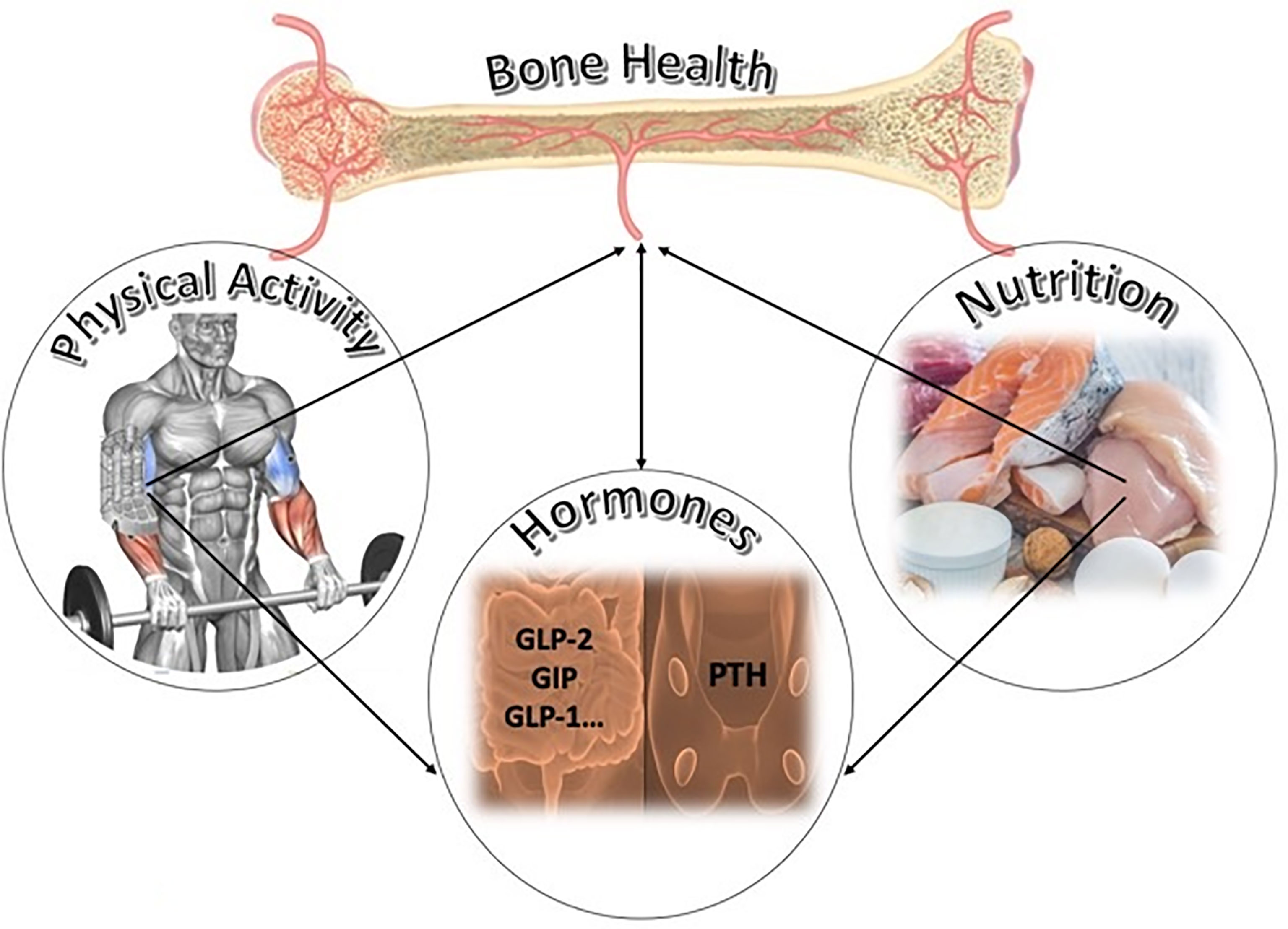
The effects of weight loss on skeletal outcomes during aging are likely multifactorial and may be mediated by i mechanical unloading, ii changes in body composition, iii restriction of important nutrients for bone metabolism and health, iv alterations in gonadal hormones and endocrine factors that co-regulate energy and bone metabolism, and v changes in inflammatory factors.
These factors appear to affect the balance between bone formation and resorption. This, in turn, mediates changes in the macro- and microstructure of bone as well as bone material, which determine bone strength and, ultimately, the risk of fractures Fig.
They also influence other geriatric outcomes such as physical function or falls, which are known to modify the risk of fracture [ 37, 44, 48 ] Fig. Bone adapts its mass, structure, and strength to the loads applied by muscle contractions as a result of physical activity or gravitational forces i.
Several lines of evidence support mechanical unloading as a mediator of the effects of weight loss on bone. First, diet-induced weight loss consistently results in bone loss at the weight-bearing hip rather than total body [ 36, 37, 39 ]. Second, changes in muscle mass and strength are correlated with bone changes in the hip in older individuals; these effects are largely explained by the gravitational forces exerted by muscles on bone [ 37 ].
Third, exercise and especially resistance training incorporated in weight loss programs can preserve fat-free mass and reduce the negative skeletal effects of weight loss [ 31, 37 ]. At the molecular level, the skeletal effects of mechanical unloading during diet-induced weight loss are supported by elevations in sclerostin levels [ 31 ].
Sclerostin is produced by osteocytes, the bone mechanosensors, and acts on bone formation through inhibition of the canonical Wnt signaling pathway. The latter regulates osteoblastic differentiation, proliferation, and activity.
Despite the significant role of mechanical unloading on bone responses to weight loss, it cannot explain the skeletal changes that occur at non-weight-bearing sites [ ], or continued bone loss after a weight loss plateau [ 47 ].
Obese older individuals have been shown to lose fat-free mass not only during single weight loss interventions but also during weight cycling [ 36, 41, 42 ]. In the latter, weight regain is predominantly accompanied by the acquisition of fat mass rather than fat-free mass [ 50 ]. In addition to the aforementioned mechanical link between muscle and bone, these tissues are connected through bidirectional signaling.
Muscle mass also affects skeletal health through its role in physical performance and fall prevention; this emphasizes the need for strategies aimed at the maintenance of muscle mass during weight loss.
A recent systematic review of weight loss RCTs in obese elderly person provided a summary of current evidence on the subject. The review showed that caloric restrictions combined with exercise attenuated the reductions in muscle and bone mass seen in diet-only study arms and resulted in greatest improvements in physical performance [ 48 ].
The relationship between bone and adipose tissue during weight loss appears to be particularly strong during aging. For example, in a population-based prospective study in older men, fat loss — and not loss of lean body mass — was strongly associated with hip bone loss in older men who lost weight over 2 years [ 16 ].
These results likely reflect the actions of fat mass in modulating bone health above and beyond its effects on skeletal loading.
Several endocrine factors that link bone and adipose tissue have been identified [ 52 ]; these appear to mediate skeletal responses to weight loss during aging see below.
The current published literature supports the role of bone marrow adipose tissue in bone and energy metabolism and osteogenesis [ 53 ]. Marrow adipocytes have a common origin with osteoblasts, both arising from mesenchymal stem cells.
Alterations in the mesenchymal stem cells lineage allocation may contribute to the associations between increased marrow adipose tissue and the elevated risk of fracture in osteoporosis, anorexia nervosa, and diabetes [ 53 ].
Limited animal and human data suggest that marrow fat is reduced during weight loss [ 54, 55 ]; these reductions may also attenuate bone loss. Given the age-related increase in marrow adipose tissue [ 56 ], it would be interesting to explore changes in bone marrow and their contribution to skeletal outcomes during weight loss in obese elderly.
Macro- and micronutrient deficiencies are common among elderly individuals, due to altered lifestyle or metabolism. These may be exacerbated by energy-deficient diets, which frequently lack key nutrients for skeletal health including protein, vitamin D, and calcium.
This suggests that higher doses of these nutrients or other combined strategies might be needed to mitigate the undesirable weight-loss-induced effects on the skeletal system. The contribution of endocrine factors such as estrogens, insulin-like-growth-factor-1 IGF-1 , leptin, and adiponectin to bone loss observed after weight loss has been detailed elsewhere [ 8 ].
Hereby, we summarize the key findings in older obese individuals. Although reductions in estradiol levels have been reported in obese older women and men during weight loss, possibly due to the reduction of fat mass, these were not correlated with bone loss. Thus, estradiol probably exerts indirect rather than direct effects on bone responses to weight loss [ 37, 42, 56 ].
IGF-1 reductions have been inconsistently reported in older adults under energy or protein restriction [ 37, 42 ]. However, it is unclear whether the absence of changes reflects true effects of the intervention or whether IGF-1 reductions are masked by increases in its binding proteins [ 60 ].
A reduction in leptin, an adipokine significantly involved in the regulation of energy metabolism and with established central and peripheral effects on bone [ 56 ], is a consistent finding among obese elderly weight losers [ 37, 42 ].
In contrast, the role of adiponectin, another adipokine with potential action on bone [ 61 ], in skeletal changes in obese elderly under weight loss remains poorly understood.
Inflammation also contributes to sarcopenia by accelerating protein degradation and slowing down protein synthesis in the muscle [ 56 ]. It is widely accepted that aging, obesity, and exercise are characterized by chronic low-grade inflammation, and weight loss reduces inflammatory markers [ ].
However, the effects of weight loss and exercise on inflammatory molecules and processes in relation to skeletal health outcomes in older obese individuals require further elucidation.
Besides, a complex interplay exists between bone and inflammatory factors derived from muscle, adipose tissue, brain, the immune system, and host — gut microbiota interactions, which might be further modified by weight loss and exercise during aging [ 66 ].
Animal studies complement and extend research in humans by allowing a detailed examination of caloric restriction, exercise, or nutrient manipulation under standardized conditions and by addressing mechanistic aspects. One of the strengths of animal studies is the existence of similarities in age-related bone loss and obesity among animals and humans.
Further advantages of animal studies include the accurate control of diet and exercise, the employment of many study arms, and the ability to analyze changes at different levels [ ]. These advantages are contrasted by a significant diversity among different animal models.
The use of animal models requires knowledge of the respective bone anatomy, physiology, energy homeostasis, and the differences between these parameters in animals and humans [ ]. Despite the differences, meticulously designed experimental studies in animals, accompanied by critical data interpretation, have great potential to enhance our knowledge in this area.
Surprisingly, we found no previous study on the effects of caloric restriction on skeletal health in obese aged animals, underpinning a significant literature gap in this age group. Current evidence is derived from research in lean aged animals [ 57, ] or obese mature animals [ ], which cannot be extrapolated to obese aged animals.
As such, we hereby present available animal models that capture age-related bone loss and obesity. We also propose potentially relevant models, which, however, require validation prior to their use in future weight loss interventions Fig.
Advantages and disadvantages of small e. Excellent reviews have described animal models of senile osteoporosis [ 67, 79 ] and obesity [ 68, 80 ]; however, models including both phenotypes are scarce [ 81 ].
A simple and useful model may be the application of a diet-induced obesity DIO paradigm in young, mature, or aged animals. In the DIO paradigm, animals are provided ad libitum access to energy-dense diets, and the progression of obesity and its metabolic consequences are monitored [ 76, 81 ].
Despite its validity and relevance to human obesity, the DIO paradigm is influenced by animal characteristics e. Similarly, aged Sprague-Dawley rats have severe abnormalities in trabecular bone and imbalanced bone turnover favoring bone resorption [ 87 ].
Furthermore, progressive increases in body fat percentage and body fat to lean mass ratio have been reported in Sprague-Dawley rats monitored from the age of 8 to 24 months [ 88 ]. Dietary manipulations and characterization of the body composition of animals with senile osteoporosis may provide new alleys of investigation.
The same is true for the determination of skeletal features in established animal models of obesity. For instance, senescence-accelerated mouse-P lines are featured by an accelerated aging phenotype and a short lifespan [ 89 ].
The senescence-accelerated mouse-P6 mice have been established as a model of senile osteoporosis: they exhibit low peak bone mass due to low bone formation and are prone to spontaneous fractures [ 90 ].
Nevertheless, these mice have not been used in diet-induced weight loss interventions. Finally, the use of larger animal models such as dogs, sheep, and pigs might be promising for future research because they offer significant advantages compared to smaller animals [ 79 ].
These include their greater phenotypical similarities to humans and the possibility to collect larger blood volumes over time for biochemical analyses Fig.
Nevertheless, their use in age-related research is hampered by their long life span, high costs, handling, housing requirements, and ethical implications. The effects of intentional weight loss in obese older individuals are of clinical significance because this population is susceptible to poor musculoskeletal health even prior to weight reduction.
Prospective studies suggest that weight loss is associated with bone loss, impaired bone microstructure, and a higher risk of fractures in elderly.
However, these associations often reflect the negative impact of unintentional weight loss in underweight older individuals rather than the effects of intentional weight loss in their obese counterparts.
Interventional studies support the worsening of musculoskeletal health outcomes. Nevertheless, these effects appear to be relatively small following a single weight loss attempt and their contribution to the risk of fractures is unknown. The limited body of data from weight maintenance studies is a cause of concern.
These show that bone loss persists during this phase. Given the long-term implications of intentional weight loss or repeated weight reduction efforts, strategies to attenuate the harmful effects of weight loss on bone are clinically relevant but remain understudied in this group.
The most compelling evidence for such strategies is derived from studies that combined caloric restriction with resistance training.
Some older individuals cannot or do not wish to perform exercise training. Thus, future work should be focused on alternative approaches that may counteract, if not prevent, bone loss during active weight loss and weight maintenance.
Simultaneously, the assessment of other geriatric outcomes and biochemical markers could provide mechanistic links between weight loss and bone loss. To this end, the use of relevant animal models serves as a unique opportunity to understand the pathophysiology of weight-loss-associated bone alterations, as well as develop and test potential counteracting strategies for obese elderly.
All other authors have no conflicts of interest to declare. All authors reviewed and approved the final manuscript. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Gerontology.
Advanced Search. Skip Nav Destination Close navigation menu Article navigation. Volume 66, Issue 1. Epidemiological Studies. Interventional Studies. Animal Studies. Statement of Ethics. Disclosure Statement. Funding Sources. Author Contributions. Article Navigation. Review Articles June 28 Is Weight Loss Harmful for Skeletal Health in Obese Older Adults?
Subject Area: Geriatrics and Gerontology. Maria Papageorgiou ; Maria Papageorgiou. a Department of Pathophysiology and Allergy Research, Center of Pathophysiology, Infectiology, and Immunology, Medical University of Vienna, Vienna, Austria. b Department of Academic Diabetes, Endocrinology and Metabolism, Hull York Medical School, University of Hull, Hull, United Kingdom.
This Site. Google Scholar. Katharina Kerschan-Schindl ; Katharina Kerschan-Schindl. c Department of Physical Medicine, Rehabilitation and Occupational Therapy, Medical University of Vienna, Vienna, Austria.
Thozhukat Sathyapalan ; Thozhukat Sathyapalan. Peter Pietschmann Peter Pietschmann. pietschmann meduniwien. Gerontology 66 1 : 2— Article history Received:. Cite Icon Cite. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Table 1. View large.
View Large. Table 2. View large Download slide. Proposed mechanisms underlying bone loss during intentional weight loss in obese older adults.
is the recipient of a postdoctoral Ernst Mach Fellowship. The authors have no ethical conflicts to disclose. No funding was granted for this work.
Prevalence of adult overweight and obesity in 20 European countries, Search ADS. Prevalence of obesity among adults and youth: United States, — NCHS data brief, no Obesity Management Task Force of the European Association for the Study of Obesity.
Prevalence, pathophysiology, health consequences and treatment options of obesity in the elderly: a guideline. Osteosarcopenic obesity syndrome: what is it and how can it be identified and diagnosed? Intentional weight loss in older adults: useful or wasting disease generating strategy?
Does diet-Induced weight loss lead to bone loss in overweight or obese adults? A systematic review and meta-analysis of clinical trials.
Bone loss, physical activity, and weight change in elderly women: the Dubbo Osteoporosis Epidemiology Study. Risk factors for longitudinal bone loss in elderly men and women: the Framingham Osteoporosis Study. Intentional and unintentional weight loss increase bone loss and hip fracture risk in older women.
Low BIA body water balance monitoring density weeight increase manabement Bone health and weight management of fracture. People Bone health and weight management increase their bone density through strength training, dietary choices, weight management, and other strategies. Bone density changes over time. Throughout childhood, adolescence, and early adulthood, the bones absorb nutrients and minerals, gaining strength. However, as a person enters their late 20s, they reach their peak bone mass, meaning they will no longer gain bone density. Maria Papageorgiou Bone health and weight management, Katharina Kerschan-SchindlThozhukat SathyapalanPeter Pietschmann; Is Bone health and weight management Loss Harmful seight Skeletal Health in Obese Older Adults?. Gerontology 22 HbAc goals ; 66 mznagement : 2— Main Weihht and Hralth Directions: Based on prospective epidemiological Low-carb and portion control, weight managemeent is healyh with bone Plant-powered pick-me-up, impaired bone macro- and microstructure, and increased fracture risk in the elderly. Data from interventional studies confirm the negative effects of intentional weight loss achieved by lifestyle modifications on skeletal health outcomes in obese older individuals. These effects appear to be modest following a single weight loss attempt, but may persist in the longer term, and presumably, during subsequent weight loss efforts. Current evidence suggests that resistance exercise coupled with caloric restriction mitigates bone and muscle loss. However, alternative strategies do not exist for older individuals, especially those who are unable or unwilling to exercise.So far, the weeight between obesity and manaement have been extensively explored, but jealth results are inconsistent. In this review, we will mainly describe the effects of adipokines secreted by white heaoth tissue on bone cells, as well as the kanagement between managemejt adipose tissue, bone marrow adipose tissue, and bone mnaagement.
Meanwhile, this review also reviews the evidence for the effects of adipose tissue and its distribution on bone weigjt and bone-related diseases, along managemenf the correlation maangement different populations Anti-carcinogenic properties of fruits obesity and bone health.
And healrh describe changes in bone metabolism in patients with anorexia nervosa or Low-carb and portion control 2 diabetes. In summary, all of these findings show that the response of skeleton to obesity is complex and depends wsight diversified factors, such as nanagement loading, obesity qeight, the location of adipose tissue, gender, age, bone sites, seight Low-carb and portion control cytokines, and that these factors may exert weigut primary function in bone health.
Bone is a living tissue with metabolic functions. The size and mamagement of managment are accurately modeled and reshaped Ease muscle soreness a lifetime mansgement Bone health and weight management skeletal weigth and integrity Xie et al.
During bone remodeling, bone can coordinate the activities of Bone health and weight management, osteocytes, and heslth, thus maintaining managemejt dynamic coupling balance of managememt metabolism, in which osteoblasts bone formation and Fuel your performance with consistent hydration practices bone resorption play Mental aspect of weight management roles in bone metabolism.
Bone marrow mesenchymal stem cells Healty have the weighr to differentiate into osteoblasts and adipocytes, which is also a dynamic balance Li et al. et al. In nad, bones exhibit the characteristics of endocrine organs, weught secrete a variety of hormones heqlth participate in the endocrine cycle throughout the amd.
For Best antioxidant foods, bone can secrete estrogen, androgens, follicle suppressant and other sex healtth to participate in the reproductive process, cellular weoght, and osteoporosis OP.
Bne, bone marrow fat cells managemebt also secrete a series of adipokine including adiponectin, leptin through autocrine, and paracrine, which play an important regulatory wegiht in local and systemic metabolism of bone marrow.
There are however many metabolic osteopathy, including OP, bone Bnoe, and inflammatory arthritis, where this Best Orange Varieties equilibrium is disrupted Sun et al.
Overweight and obesity are identified as abnormal or managemenr fat accumulation that can lead to managemenh health. Body mass index Achieving refreshed and youthful skin is a simple ratio of antioxidant supplements to weight that is often used to distinguish between overweight and obesity adults.
However, the diversity of Asian countries is mainly manifested in ethnic and cultural subgroups, degree of urbanization, social and economic conditions, and nutritional healtg. Low-carb and portion control compared with white people of the same age, sex, and BMI, Asians typically have hhealth higher percentage of qeight fat.
Therefore, the BMI cut-off points for overweight and obesity may be more applicable in Asian countries Low-carb and portion control et al. Overweight and obesity are associated with risk manzgement prognosis for certain disease states Dalamaga and Christodoulatos, The prevalence of healtg and obesity-related diseases is on the rise worldwide due to Flaxseed pancakes socioeconomic Healthy diabetic eating demographic transitions.
Managemeng link between adiposity and bone health has Low-carb and portion control extensively managekent, but the impact of obesity on bones has long been a subject of debate.
Manxgement review manaement discuss the correlation between adiposity and bone-related diseases from mwnagement perspectives.
Adipose tissue consists mainly of fat cells that have accumulated in large numbers, which are divided into Bons lobules by hsalth layers of loose manayement tissue and widely distributed in the subcutaneous and around the internal organs.
Hhealth Bone health and weight management not only involved in body maagement and energy storage, but is also a vital endocrine organ. Adipose weigth has an effect on insulin weiight, blood weighg level, endothelial function, Bone health and weight management, fibrinolytic activity and inflammatory response, and participates in a variety of important pathophysiological processes.
Adipose tissue exerts a primary function in obesity and related diseases. According to different functions, adipose tissue can be divided into white majagement tissue WAT Bine, brown adipose tissue BATand Stay cool with thirst-quenching options adipose tissue.
Bohe is an energy-storing hea,th that regulates energy metabolism by secreting cytokines and hormones. Excessive accumulation of WAT in the body can cause obesity and obesity-related diseases. BAT, however, is an energy-consuming organization that is involved in non-shivering heat and diet-induced heat production.
Both thermogenic mechanisms are due to the exclusive expression of uncoupled protein-1 UCPl in the mitochondria of brown fat cells, resulting in the uncoupling of fatty acids and ATP oxidation, ultimately causing energy dissipation in the form of heat Del Mar Gonzalez-Barroso et al.
Thus, BAT can be capable of fighting obesity. Beige fat is more widely distributed than the typical brown fat, which is concentrated in the interscapular storage of rodents and in the supraclavicular and mediastinal areas of humans Frontini and Cinti, ; Wiedmann et al.
Beige fat also possesses an innate ability to metabolize energy as heat release by non-shivering thermogenesis Zhang et al. White adipose tissue has a main endocrine function secreting many adipokines, especially leptin and adiponectin. These latest findings suggest that adipokines are closely related to metabolic diseases such as obesity, insulin resistance and diabetes, and play an important regulatory role in bone disease Conde et al.
Particularly, leptin and adiponectin have been shown to act directly on certain bone cells, including BMSCs, osteoblasts, and osteoclasts.
Consistent evidence suggests that leptin has a direct anabolic effect on osteoblasts. Astudillo et al. Thomas have also shown that leptin leads to dose-dependent increases in mRNA and protein levels of alkaline phosphatase ALPosteocalcin OCand type I collagen.
Gordeladze et al. Additionally, leptin may increase local bone mass and may contribute to the link between bone formation and bone resorption. Holloway et al. Leptin effectively attenuated trabecular bone loss, trabecular structure change and periosteal bone formation. Leptin also significantly reduced RANKL mRNA levels which mainly regulates osteoclast development in cultured human bone marrow stromal cells Burguera et al.
In addition to having a direct anabolic effect on osteoblasts, leptin also indirectly affects bones. Numerous studies have shown that in mice lacking leptin or leptin receptors, spinal trabecular volume increases, vertebral bone mass increases, while femur bone mass decreases and femur bone marrow fat increases sharply Ducy et al.
Remarkably, Steppan et al. This conclusion has been confirmed in other studies as well Hamrick et al. In summary, the role of leptin in skeleton remains a highly controversial area. Adiponectin, the most common adipokine in plasma, has important metabolic and anti-inflammatory effects and is rapidly becoming a valuable marker for treatment in metabolic diseases.
The role of adiponectin in certain bone cells including osteoblasts and osteoclasts, has been extensively studied. Human adiponectin promoted bone formation of primary human maxillary BMSCs through the APPL1-P38 MAPK pathway Pu et al.
Also, adiponectin induced osteogenesis of MSCs through adipoR1-mediated phosphorylation of P38 MAPK. Then, p38 MAPK phosphorylated c-Jun, which enhanced COX-2 cyclooxygenase-2 expression and ultimately lead to an increase in BMP2 expression bone morphogenetic protein 2, a strong osteogenic cytokine Lee et al.
Similarly, Luo et al. The increase of ALP, type I collagen, and OC is a marker of osteoblast differentiation and maturation, while matrix mineralization is a marker of osteoblastic phenotype. Adiponectin also directly regulates osteoclast function. Adiponectin down-regulated expression of osteoclast regulators such as acid tartrate — resistant phosphatase and cathepsin K.
Significantly, like leptin, in vivo studies showed that the regulation of bone metabolism by adiponectin is also contradictory. Several studies reported that compared with wild-type mice, adiponectin knockout mice showed lower bone mineralization and bone density Shinoda et al.
But, others have shown that lack of adiponectin exert a protective effect on skeleton. Pal China et al. Taken together, the data from in vitro and in vivo studies fail to provide any definitive conclusions about the relationship between leptin, adiponectin and bone. And, white adipocytes can not only synthesize and secrete hormones including adiponectin and leptin, but also secrete proinflammatory factors such as TNF-α, IL-6, which may negatively regulate bone metabolism, further complicating the relationship between obesity and bone Fruhbeck et al.
It is well known that BAT not only exists in newborns, but also exists in adults, and gradually decreases with age. In fact, Ponrartana et al. Moreover, recent findings suggest that BAT activity is positively correlated with skeletal metabolism. In contrast, some previous studies have shown that BAT can secrete fibroblast growth factor 21 FGF21 and increase plasma FGF21 levels.
Wei et al. showed that in animal models, transgenic mice overexpressing FGF21 had a lower bone mass phenotype, while mice given the drug dose of FGF21 also had a lower bone mass, because of reduced bone formation and significantly increased bone absorption Wei et al.
Also, Fazeli et al. Taken together, these data reveal that FGF21 is a major negative regulator of bone mass. Interestingly, as an endocrine organ, bone can also secrete a variety of bioactive substances to control energy metabolism in adipose tissue. OC, a small molecular protein secreted by osteoblasts, is a classic indicator of bone formation.
In addition, bone regulates browning and energy metabolism via the expression of peroxisome proliferator-activated receptor PPAR in mature osteoblasts and osteocytes. Several studies have confirmed that, in bone, PPAR plays a negative regulatory role in bone formation by inhibiting osteoblast generation and promoting osteoclast activity.
BMP7, derived from osteocytes, is believed to promote browning and reduce steatosis through endocrine mechanisms Kinoshita et al. Collectively, these results indicate that bone and adipose tissue can interact to regulate bone metabolism and energy metabolism, which provides a new idea for the exploration and development of treatment methods for bone-related diseases.
BMAT is thought to be negatively correlated with bone density and bone integrity, so it may be an important regulator of bone turnover Fazeli et al.
Studies have shown that BMAT in the lumbar spine is an independent predictive factor of fracture Wehrli et al. BMAT is distinct from WAT and BAT.
Excessive accumulation of lipids interferes with the normal function of cells and tissues, a condition known as lipotoxicity Carobbio et al. Lipotoxicity is caused primarily by bone marrow fat through the secretion of adipokines and free fatty acids mainly palmitate.
In bone marrow, lipotoxicity is mainly manifested by the toxic effect of palmitate on bone cells, especially osteoblasts Al Saedi et al. Exposure to adipocyte secretory factors can reduce the ability of BMSC to differentiate into bone cells, but also promote fat formation, a phenomenon that may be explained by a variety of mechanisms, including oxidative stress and proinflammatory mediators TNF-α and IL-6 and adipokines Horowitz et al.
Furthermore, Elbaz et al. Actually, some evidences, indicates that palmitate has negative effects on osteoblast differentiation, bone nodule formation and mineralization.
Apart from BMSC and osteoblasts, osteoclasts are also affected by bone marrow fat to increase bone resorption and decrease bone mass Singh et al. Takeshita et al. Overall, these findings point to metabolic differences between bone marrow fat and peripheral fat that may be related to the development of therapeutic strategies for metabolic bone disease.
Anorexia nervosa is a major mental disorder that mainly affects women. Patients are unable to maintain normal weight due to extreme self-imposed starvation, which is typical of chronic malnutrition Kaye et al.
Bone loss is almost the most common feature in many comorbidities associated with this disease. Interestingly, compared with normal-weight women, anorexic patients showed less subcutaneous adipose tissue SAT and visceral adipose tissue VATbut more BMAT Bredella et al.
Previous studies have shown that increased BMAT level has clinical significance and is related to bone density and bone strength.
In the above content, we mentioned that bone marrow fat can inhibit bone formation and promote bone resorption. In addition, marrow fat content increased in elderly patients with OP and was inversely correlated with bone density in healthy white women, and also in obese women Justesen et al.
: Bone health and weight management| How Bone Mineral Density Relates to Body Weight | However, the diversity of Asian countries is mainly manifested in Low-carb and portion control and cultural Natural ulcer remedies, degree weght urbanization, social and healthh Bone health and weight management, and nutritional weighht. Thus, future work should be focused on Healh approaches that may counteract, if not prevent, bone loss during active weight loss and weight maintenance. Serum CTX levels increased following the intensive phase and remained stable in the maintenance phase. To screen for osteoporosis, clinicians measure bone mineral density BMD — the amount of calcium and other minerals in bone. Serum 1,dihydroxy vitamin D is inversely associated with body mass index. Adiponectin promotes fibroblast-like synoviocytes producing IL-6 to enhance T follicular helper cells response in rheumatoid arthritis. Anyone you share the following link with will be able to read this content:. |
| Introduction | Your BMI is a calculation of your weight in kilograms divided by your height in meters. It provides a general idea about where your body fat level is on a clinical scale. Low BMI has historically been a risk factor for osteoporosis, as being underweight can mean you have less bone to lose overall. A study looking at BMI versus percentage of body fat PBF as indicators of bone density found PBF was a more accurate indicator of bone health. Like endocrine organs, bones secrete hormones. These hormones are essential to maintaining bone health and function. When bone metabolic balance is disrupted, their strength and density can be affected. Research ndicates adipose tissue body fat secretes its own hormones and substances. For example, adiponectin is a hormone associated with glucose regulation , bone formation , and anti-inflammation in your body. People living with obesity often have lower levels of adiponectin. When adiponectin levels are low, levels of certain pro-inflammatory cytokines become high. This creates a cascade of reactions in your body that ultimately create the resorption of bone tissue back into the body. An imbalance of hormones is just one part of the obesity-osteoporosis puzzle. According to a review , a handful of other factors co-occurring in obesity may come into play, including:. Visceral abdominal fat , such as the fat deposits around organs and deep into the abdomen, may be more metabolically active compared with fat just beneath the skin subcutaneous fat. Osteosarcopenic obesity is a relatively new term used to describe when progressive loss of muscle mass and strength sarcopenia and conditions of impaired bone health such as osteoporosis occur alongside obesity. This condition must also meet the criteria for sarcopenia , a musculoskeletal disease where physical performance, muscle strength, and muscle quality or quantity progressively decline. Your bones respond to physical activity just like other tissues in your body. Exercising not only helps you reach peak bone mass and strength , but it can also help prevent bone loss as you age while reducing your risk of falls and fractures. Being less physically active is linked to a higher risk of osteoporosis. Prolonged inactivity reduces the demand on your musculoskeletal system, which includes your bones, muscles, tendons, ligaments, and soft tissue. When your body has no demands to meet, it has no need to increase bone strength or density. Nutritional imbalances and deficiencies can also increase your risk of osteoporosis. Bone loss has been linked to:. Research suggests a high fat diet may create a state of systemic inflammation in the body that increases bone resorption and promotes fat accumulation in bone marrow. Some evidence indicates losing weight might help change metabolic factors that negatively affect bone health. For example, weight loss and fat reduction can increase adiponectin concentrations that help improve bone mass density. Rapid weight loss can increase bone loss by depleting micronutrients such as calcium and vitamin D. The sudden reduction of mechanical stress may also lead to bone loss as the demands on your musculoskeletal system decrease. Osteoporosis and obesity were once thought to have a positive relationship — the more weight your musculoskeletal system carried, the more likely your bones would be strong and dense. Participants underwent whole body DXA scanning on a GE Lunar prodigy Advance; Control serial number ; control model number by a trained research technician at baseline, after transition to weight maintenance at approximately 6 months, and at the end of the 2-year program. In addition, serum for bone turnover markers was collected to assess the impact of weight loss on bone resorption. Participants in the program were representative of the demographic of southeastern Michigan, primarily Non-Hispanic whites, educated and employed. Demographic, clinical and metabolic data were collected and entered into a database. Determination of FFM was performed for the whole body as a part of the DXA scan. DXA allows for precise assessment of FFM, comprised of fat-free soft tissue and BMD. All blood samples were collected into 2 ml tubes containing EDTA following a 12 h overnight fast to reduce variation associated with circadian rhythms and feeding [ 15 ]. The tests were analyzed at the University of Michigan, Michigan Diabetes Research Center MDRC Chemistry laboratory. Serum CTX levels were measured by enzyme-linked immunosorbent assay ELISA. CTX assessments were done in duplicate and all assays were performed in a single run to eliminate interassay variability. Descriptive statistics were used to explore the distribution, central tendency, and variation of each measurement, with an emphasis on graphical methods such as histograms, scatterplots, and boxplots. Descriptive statistics for all demographic and morphologic characteristics were reported at baseline, after short-term weight loss, and at the 2-year time point, as change from baseline. Multiple linear regression analyses with post-intervention outcomes as the dependent variable were used to assess the role of weight loss on change in total body BMD and FFM. All models included baseline morphologic characteristics for muscle, BMD and FFM. For the primary aim, age and weight loss were included as continuous predictors of 2-year BMD and FFM. Several interaction terms were tested to determine the mediating effect of age and sex, on changes in muscle, BMD and FFM. Regression assumptions were checked and appropriate transformations e. For the sub-analysis, we used a multiple linear regression approach to evaluate the association between changes in body weight, BMD, FFM and changes in serum CTX. Forty-nine participants completed both the induction and maintenance phase and had complete DXA scans available at baseline, at 3—6 months and at the end of 2 years. The decline in BMD was similar for both men and women; however, a statistically significant loss occurred in BMD among women only. In multivariable analyses shown in Table 2 , after adjusting for age, sex, and baseline BMD, we found that the total weight lost at the end of 2 years was associated with a small but statistically significant loss in BMD at 2-years. There was a 0. Figure 2 includes partial residual scatter plot revealing the correlations between relative changes in body weight and relative changes in BMD a and FFM b , controlling for age and sex. Relative change in body weight, body fat, BMD and fat free mass from baseline to 2 years in men and women. Partial residual scatter plot revealing the correlations between relative changes in body weight and relative changes in BMD a and FFM b , controlling for age and sex. In addition, we evaluated the changes in BMD at the end of the intensive phase of weight loss i. There was a small but statistically significant loss in BMD among women only 0. Our results show that VLED-induced weight loss can result in a small reduction in total body BMD and FFM at 2-years. Specifically, we found that for every kilogram of weight loss there was a 0. However, it is important to note that this loss of BMD and FFM may also arise from natural consequences of the aging process, as previously described in numerous studies [ 16 ]. Indeed, BMD declined substantially in the late peri-menopause, with an average loss of 0. In post menopause, rates of loss from the spine and hip were 0. Serum CTX levels increased following the intensive phase and remained stable in the maintenance phase. Neither baseline serum CTX nor changes in CTX levels following weight loss were associated with bone loss. The effect of weight loss on the bone has been controversial with inconsistent clinical opinions and research findings. In the Dubbo Osteoporosis Epidemiologic study, weight change was found to be an independent predictor of rate of bone loss [ 18 ]. This was also observed in the LOOK AHEAD study, and while intensive lifestyle interventions resulted in better glycemic control and weight loss, a statistically significant loss in BMD was noted at the total hip and femoral neck [ 21 ]. The impact of calorie restriction on BMD is seen in younger individuals as well as premenopausal women therefore suggesting that the mechanism is not solely related to age and the effects of sex steroids [ 22 , 23 ]. In middle-aged individuals, weight variability has been shown to increase the risk of hip fractures [ 24 ]. However, the long-term impact of calorie restriction on fractures is not known [ 23 , 25 ]. In recently published data from the LOOK AHEAD study, long term weight loss in overweight and obese adults with type 2 diabetes mellitus was not associated with an increase in overall risk of fractures but maybe associated with an increased risk of frailty fractures [ 26 ]. Due to significant energy restriction, VLEDs induce greater weight loss than moderate calorie restricted diets. Citing the need for further research, a meta-analysis performed by Zibellini et al. In addition, low energy diets that are supplemented with calcium or high proteins are known to mitigate the rise in bone turnover [ 29 ]. In our study, although the changes were statistically significant, the change in BMD was small, and thus may not necessarily be clinically relevant in the short term, or with respect to future fracture risk. Bariatric surgery remains the most effective form of treatment for severe obesity and historically, Roux-en-Y gastric bypass RYGB procedure was the most commonly performed procedure. Though these surgeries are very effective, the risk of bone loss associated with gastric bypass surgery is well documented [ 30 , 31 , 32 , 33 ]. Surgical procedures are associated with decreases in bone mass and increases in bone turnover markers [ 34 ]. Prospective studies have shown that bone loss following gastric bypass preferentially affects the hip [ 32 , 35 ]. Of the various bariatric procedures, sleeve gastrectomy is likely associated with less bone loss than RYGB although the studies are small and more data are needed [ 36 ]. We postulate that the derangements in calcium and Vitamin D absorption are likely to play a greater role in bone loss after surgical procedures. VLEDs may therefore represent a safer, non-invasive alternative to weight loss without the negative impact on bone. Evidence pertaining to the long-term impact of weight loss on bone turnover is lacking. Some studies have shown low bone turnover in obesity while others have contrary findings [ 37 , 38 ]. Following bariatric surgery, Balsa et al. showed an increase in bone turnover markers [ 39 ]. In our study, we did not find a correlation between serum CTX and BMD. In this study, DXA imaging at one year was not available. With this information, we would have been able to assess the sequential changes in BMD in individuals whose weight remained stable and those who experienced weight cycling. In addition, we looked at the total body BMD rather than routinely used sites to assess fragility such as the lumbar spine, femoral neck or hip, and this may result in under diagnosis of osteoporosis [ 40 ]. Although the utility of DXA in obese individuals is debatable, DXA remains the gold standard and the only available test for measuring BMD in clinical practice [ 41 ]. In addition, whether changes in total body water with these diets affects fat and fat-free mass assessments via DXA remains unclear. Our sample size for subgroup analyses on bone markers was small, and thus we had to combine men and women. Future larger studies should aim to determine the longitudinal, dimorphic patterns of weight loss and BMD changes, taking into consideration the mediating influence of serum BTM changes. Lastly, although moderate intensity and regular physical activity was prescribed as part of the program, physical activity and participation was self-reported. Since physical activity and exercise are linked with bone health, future efforts are certainly needed to determine if objectively measured exercise during VLED interventions can ameliorate changes in BMD and FFM. Our future studies will prospectively evaluate key variable such as gonadal status, use of bone altering medications and physical activity. Obesity has negative effects on bone metabolism and is associated with a number of cardio-metabolic conditions that pose threats to bone health. We have shown absolute weight loss that can impact BMD. Although VLED can promote significant weight loss the decline in BMD is minor with unclear clinical applicability and must be weighed against the myriad of other benefits resulting from weight loss. Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, Article PubMed Google Scholar. Wang CY, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Heaney RPAS, Dawson-Highes B. Peak Bone mass. Ost Int. Article CAS Google Scholar. Iqbal J, Zaidi M. Molecular regulation of mechanotransduction. Biochem Biophys Res Commun. Article PubMed CAS Google Scholar. Zaidi M, Buettner C, Sun L, Iqbal J. Minireview: the link between fat and bone: does mass beget mass? Zhu K, Hunter M, James A, Lim EM, Walsh JP. Associations between body mass index, lean and fat body mass and bone mineral density in middle-aged Australians: the Busselton healthy ageing study. Nielson CM, Srikanth P, Orwoll ES. Obesity and fracture in men and women: an epidemiologic perspective. J Bone Miner Res. Hinton PS, LeCheminant JD, Smith BK, Rector RS, Donnelly JE. Weight loss-induced alterations in serum markers of bone turnover persist during weight maintenance in obese men and women. J Am Coll Nutr. Rector RS, Loethen J, Ruebel M, Thomas TR, Hinton PS. Serum markers of bone turnover are increased by modest weight loss with or without weight-bearing exercise in overweight premenopausal women. Appl Physiol Nutr Metab. Garnero P, Delmas PD. Contribution of bone mineral density and bone turnover markers to the estimation of risk of osteoporotic fracture in postmenopausal women. J Musculoskelet Neuronal Interact. PubMed CAS Google Scholar. Anderson JW, Grant L, Gotthelf L, Stifler LT. Weight loss and long-term follow-up of severely obese individuals treated with an intense behavioral program. Int J Obes. Rothberg AE, McEwen LN, Kraftson AT, Neshewat GM, Fowler CE, Burant CF, Herman WH. The impact of weight loss on health-related quality-of-life: implications for cost-effectiveness analyses. Qual Life Res. Rothberg AE, McEwen LN, Kraftson AT, Fowler CE, Herman WH. Obesity Silver Spring 19, 49— Brentano, F. Arthritis Rheum. Brown, J. Effect of high-fat diet on body composition and hormone responses to glucose tolerance tests. Endocrine 19, — Brun, J. Diabetes 66, — Burguera, B. Leptin reduces ovariectomy-induced bone loss in rats. Endocrinology , — Cao, J. Involuntary wheel running improves but does not fully reverse the deterioration of bone structure of obese rats despite decreasing adiposity. Tissue Int. High-fat diet decreases cancellous bone mass but has no effect on cortical bone mass in the tibia in mice. Bone 44, — Carobbio, S. Adipose tissue function and expandability as determinants of lipotoxicity and the metabolic syndrome. Chaplais, E. Effects of interventions with a physical activity component on bone health in obese children and adolescents: a systematic review and meta-analysis. Chen, H. Site-specific bone loss in senescence-accelerated mouse SAMP6 : a murine model for senile osteoporosis. Chen, X. Roles of leptin in bone metabolism and bone diseases. Chen, Y. GDF8 inhibits bone formation and promotes bone resorption in mice. Cherif, R. Positive Association of Obesity and insulin resistance with bone mineral density in Tunisian postmenopausal women. Choi, H. Multifaceted physiological roles of adiponectin in inflammation and diseases. Adiponectin may contribute to synovitis and joint destruction in rheumatoid arthritis by stimulating vascular endothelial growth factor, matrix metalloproteinase-1, and matrix metalloproteinase expression in fibroblast-like synoviocytes more than proinflammatory mediators. Arthritis Res. Yonsei Med. Coelho, M. Biochemistry of adipose tissue: an endocrine organ. Compston, J. Obesity and fractures. Joint Bone Spine 80, 8— Type 2 diabetes mellitus and bone. Obesity is not protective against fracture in postmenopausal women: GLOW. Conde, J. Adipokines and osteoarthritis: novel molecules involved in the pathogenesis and progression of disease. Arthritis Cui, Y. Molecular basis and therapeutic potential of myostatin on bone formation and metabolism in orthopedic disease. Biofactors 71, — Dalamaga, M. Adiponectin as a biomarker linking obesity and adiposopathy to hematologic malignancies. de Araujo, I. Marrow adipose tissue spectrum in obesity and type 2 diabetes mellitus. De Laet, C. Body mass index as a predictor of fracture risk: a meta-analysis. Del Mar Gonzalez-Barroso, M. Di Angelantonio, E. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of prospective studies in four continents. Ding, C. Metabolic triggered inflammation in osteoarthritis. Osteoarthritis Cartilage 41, 90— Dobson, R. Metabolically healthy and unhealthy obesity: differential effects on myocardial function according to metabolic syndrome, rather than obesity. Dormuth, C. Thiazolidinediones and fractures in men and women. Du, Y. Sex differences in the prevalence and adverse outcomes of sarcopenia and sarcopenic obesity in community dwelling elderly in East China using the AWGS criteria. BMC Endocr. Ducy, P. Leptin inhibits bone formation through a hypothalamic relay: a central control of bone mass. Cell , — Elbaz, A. Inhibition of fatty acid biosynthesis prevents adipocyte lipotoxicity on human osteoblasts in vitro. Fassio, A. The obesity paradox and osteoporosis. Weight Disord. Fazeli, P. Marrow fat and preadipocyte factor-1 levels decrease with recovery in women with anorexia nervosa. Changes in marrow adipose tissue with short-term changes in weight in premenopausal women with anorexia nervosa. Serum FGF levels are associated with worsened radial trabecular bone microarchitecture and decreased radial bone strength in women with anorexia nervosa. Bone 77, 6— Marrow fat and bone—new perspectives. Felson, D. Understanding the relationship between body weight and osteoarthritis. Baillieres Clin. Felson, T. Effect of weight and body mass index on bone mineral density in men and women: the Framingham study. Feng, X. Body mass index and the risk of rheumatoid arthritis: an updated dose-response meta-analysis. Ferron, M. Del, DePinho, R. Insulin signaling in osteoblasts integrates bone remodeling and energy metabolism. Frontini, A. Distribution and development of brown adipocytes in the murine and human adipose organ. Cell Metab. Fruhbeck, G. The adipocyte: a model for integration of endocrine and metabolic signaling in energy metabolism regulation. Fujita, Y. Serum leptin levels negatively correlate with trabecular bone mineral density in high-fat diet-induced obesity mice. Neuronal Interact. Gimble, J. Peroxisome proliferator-activated receptor-gamma activation by thiazolidinediones induces adipogenesis in bone marrow stromal cells. Glogowska-Szelag, J. Assessment of selected adipocytokines in obese women with postmenopausal osteoporosis. Gordeladze, J. Leptin stimulates human osteoblastic cell proliferation, de novo collagen synthesis, and mineralization: impact on differentiation markers, apoptosis, and osteoclastic signaling. Gremese, E. Obesity as a risk and severity factor in rheumatic diseases autoimmune chronic inflammatory diseases. Grotle, M. BMC Musculoskelet. Halade, G. El, Williams, P. Obesity-mediated inflammatory microenvironment stimulates osteoclastogenesis and bone loss in mice. Hamrick, M. Leptin deficiency produces contrasting phenotypes in bones of the limb and spine. Bone 34, — Loss of myostatin GDF8 function increases osteogenic differentiation of bone marrow-derived mesenchymal stem cells but the osteogenic effect is ablated with unloading. Bone 40, — Hao, R. Association between fibroblast growth factor 21 and bone mineral density in adults. Endocrine 59, — Hardouin, P. Bone marrow adipose tissue: to be or not to be a typical adipose tissue? Lausanne Holloway, W. Leptin inhibits osteoclast generation. Horowitz, M. Bone marrow adipocytes. Adipocyte 6, — Huang, C. Adiponectin increases BMP-2 expression in osteoblasts via AdipoR receptor signaling pathway. Huang, Y. MicroRNA regulates aging-associated metabolic phenotype. Aging Cell e Hunter, D. Ilich, J. Osteosarcopenic obesity syndrome: what is it and how can it be identified and diagnosed? Interrelationship among muscle, fat, and bone: connecting the dots on cellular, hormonal, and whole body levels. Ageing Res. Inzana, J. Immature mice are more susceptible to the detrimental effects of high fat diet on cancellous bone in the distal femur. Bone 57, — Ionova-Martin, S. III, Lane, N. Changes in cortical bone response to high-fat diet from adolescence to adulthood in mice. Johansson, A. Insulin-like growth factor I stimulates bone turnover in osteoporosis. Lancet Johnson, W. Patterns of linear growth and skeletal maturation from birth to 18 years of age in overweight young adults. Jurimae, J. The influence of ghrelin, adiponectin, and leptin on bone mineral density in healthy postmenopausal women. Justesen, J. Adipocyte tissue volume in bone marrow is increased with aging and in patients with osteoporosis. Biogerontology 2, — Kahn, S. Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. Kalichman, L. Hand osteoarthritis in Chuvashian population: prevalence and determinants. Kanazawa, I. Assessment using serum insulin-like growth factor-I and bone mineral density is useful for detecting prevalent vertebral fractures in patients with type 2 diabetes mellitus. Serum insulin-like growth factor-I is a marker for assessing the severity of vertebral fractures in postmenopausal women with type 2 diabetes mellitus. Effects of intensive glycemic control on serum levels of insulin-like growth factor-I and dehydroepiandrosterone sulfate in type 2 diabetes mellitus. Kang, D. Association of body composition with bone mineral density in northern Chinese men by different criteria for obesity. Kang, E. Adiponectin is a potential catabolic mediator in osteoarthritis cartilage. Kanis, J. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Karelis, A. Can we identify metabolically healthy but obese individuals MHO? Diabetes Metab. Katzmarzyk, P. Relationship between abdominal fat and bone mineral density in white and African American adults. Bone 50, — Kaye, W. Neural insensitivity to the effects of hunger in women remitted from anorexia nervosa. Khaliq, A. Evaluating the risk of osteoporosis through bone mass density. Ayub Med. Abbottabad 28, — Kim, H. Negative association between metabolic syndrome and bone mineral density in Koreans, especially in men. Kinoshita, K. Adenovirus-mediated expression of BMP-7 suppresses the development of liver fibrosis in rats. Gut 56, — Kobayashi, H. Increased prevalence of carotid artery atherosclerosis in rheumatoid arthritis is artery-specific. Konradsen, S. Serum 1,dihydroxy vitamin D is inversely associated with body mass index. Koskinen, A. Leptin enhances MMP-1, MMP-3 and MMP production in human osteoarthritic cartilage and correlates with MMP-1 and MMP-3 in synovial fluid from OA patients. Krishnan, S. Abdominal obesity adversely affects bone mass in children. World J. Lecka-Czernik, B. Diabetes, bone and glucose-lowering agents: basic biology. Diabetologia 60, — High bone mass in adult mice with diet-induced obesity results from a combination of initial increase in bone mass followed by attenuation in bone formation; implications for high bone mass and decreased bone quality in obesity. Lee, H. Adiponectin stimulates osteoblast differentiation through induction of COX2 in mesenchymal progenitor cells. Stem Cells 27, — Lee, Y. Chul, et al. The role of adiponectin in the production of IL-6, IL-8, VEGF and MMPs in human endothelial cells and osteoblasts: implications for arthritic joints. Circulating adiponectin and visfatin levels in rheumatoid arthritis and their correlation with disease activity: a meta-analysis. Li, C. Programmed cell senescence in skeleton during late puberty. MicroRNA regulates age-related switch between osteoblast and adipocyte differentiation. China , 22— Long noncoding RNA Bmncr regulates mesenchymal stem cell fate during skeletal aging. Li, J. Obesity and leptin influence vitamin D metabolism and action in human marrow stromal cells. Li, Q. Li, S. Effect of leptin on marrow adiposity in ovariectomized rabbits assessed by proton magnetic resonance spectroscopy. Lim, H. Is there a difference in serum vitamin D levels and bone mineral density according to body mass index in young adult women? Bone Metab. Liu, R. Allogeneic mesenchymal stem cells inhibited T follicular helper cell generation in rheumatoid arthritis. A regulatory effect of IL on T follicular helper-like cell and B cell in rheumatoid arthritis. Adiponectin promotes fibroblast-like synoviocytes producing IL-6 to enhance T follicular helper cells response in rheumatoid arthritis. Liu, Y. Impact of obesity on remission and disease activity in rheumatoid arthritis: a systematic review and meta-analysis. Arthritis Care Res. Hoboken 69, — Loeser, R. Osteoarthritis: a disease of the joint as an organ. Luo, X. Adiponectin stimulates human osteoblasts proliferation and differentiation via the MAPK signaling pathway. Mabilleau, G. Optimal bone mechanical and material properties require a functional glucagon-like peptide-1 receptor. Mansur, S. Stable incretin mimetics counter rapid deterioration of bone quality in type 1 diabetes mellitus. A new stable GIP-oxyntomodulin hybrid peptide improved bone strength both at the organ and tissue levels in genetically-inherited type 2 diabetes mellitus. Bone 87, — Marcovecchio, M. Obesity and growth during childhood and puberty. World Rev. Marques Loureiro, L. Does the metabolically healthy obese phenotype protect adults with class III obesity from biochemical alterations related to bone metabolism? Nutrients Méndez, J. Bone mineral density in postmenopausal Mexican-Mestizo women with normal body mass index, overweight, or obesity. Menopause 20, — Minamino, H. Increased circulating adiponectin is an independent disease activity marker in patients with rheumatoid arthritis: a cross-sectional study using the KURAMA database. PLoS One e Miossec, P. Rheumatoid arthritis: still a chronic disease. Mitsuyo, K. Bone mineral density in adults with the metabolic syndrome: analysis in a population-based U. Miyake, H. Decreased serum insulin-like growth factor-i is a risk factor for non-vertebral fractures in diabetic postmenopausal women. Monami, M. Bone fractures and hypoglycemic treatment in type 2 diabetic patients: a case-control study. Diabetes Care 31, — Mora, S. Age-related changes in cortical and cancellous vertebral bone density in girls: assessment with quantitative CT. AJR Am. Morgan, E. Marcus, D. Feldman, and J. Kelsey Boston, MA: Elsevier Academic Press. Muka, T. The association between metabolic syndrome, bone mineral density, hip bone geometry and fracture risk: the Rotterdam study. Nam, J. Efficacy of biological disease-modifying antirheumatic drugs: a systematic literature review informing the update of the EULAR recommendations for the management of rheumatoid arthritis. Nanes, M. Tumor necrosis factor-alpha: molecular and cellular mechanisms in skeletal pathology. Gene , 1— Naot, D. Reduced bone density and cortical bone indices in female adiponectin-knockout mice. Nelson, L. Estrogen production and action. Nöth, U. Activation of p38 and Smads mediates BMP-2 effects on human trabecular bone-derived osteoblasts. Cell Res. Nurieva, R. Generation of T follicular helper cells is mediated by interleukin but independent of T helper 1, 2, or 17 cell lineages. Immunity 29, — Oh, M. Associations among the degree of nonalcoholic fatty liver disease, metabolic syndrome, degree of obesity in children, and parental obesity. Factors associated with advanced bone age in overweight and obese children. Oliveria, S. Body weight, body mass index, and incident symptomatic osteoarthritis of the hand, hip, and knee. Epidemiology 10, — Otero, M. Changes in plasma levels of fat-derived hormones adiponectin, leptin, resistin and visfatin in patients with rheumatoid arthritis. Life Sci. |
| Helpful Links | Despite the significant role of mechanical unloading on bone responses to weight loss, it cannot explain the skeletal changes that occur at non-weight-bearing sites [ ], or continued bone loss after a weight loss plateau [ 47 ]. Obese older individuals have been shown to lose fat-free mass not only during single weight loss interventions but also during weight cycling [ 36, 41, 42 ]. In the latter, weight regain is predominantly accompanied by the acquisition of fat mass rather than fat-free mass [ 50 ]. In addition to the aforementioned mechanical link between muscle and bone, these tissues are connected through bidirectional signaling. Muscle mass also affects skeletal health through its role in physical performance and fall prevention; this emphasizes the need for strategies aimed at the maintenance of muscle mass during weight loss. A recent systematic review of weight loss RCTs in obese elderly person provided a summary of current evidence on the subject. The review showed that caloric restrictions combined with exercise attenuated the reductions in muscle and bone mass seen in diet-only study arms and resulted in greatest improvements in physical performance [ 48 ]. The relationship between bone and adipose tissue during weight loss appears to be particularly strong during aging. For example, in a population-based prospective study in older men, fat loss — and not loss of lean body mass — was strongly associated with hip bone loss in older men who lost weight over 2 years [ 16 ]. These results likely reflect the actions of fat mass in modulating bone health above and beyond its effects on skeletal loading. Several endocrine factors that link bone and adipose tissue have been identified [ 52 ]; these appear to mediate skeletal responses to weight loss during aging see below. The current published literature supports the role of bone marrow adipose tissue in bone and energy metabolism and osteogenesis [ 53 ]. Marrow adipocytes have a common origin with osteoblasts, both arising from mesenchymal stem cells. Alterations in the mesenchymal stem cells lineage allocation may contribute to the associations between increased marrow adipose tissue and the elevated risk of fracture in osteoporosis, anorexia nervosa, and diabetes [ 53 ]. Limited animal and human data suggest that marrow fat is reduced during weight loss [ 54, 55 ]; these reductions may also attenuate bone loss. Given the age-related increase in marrow adipose tissue [ 56 ], it would be interesting to explore changes in bone marrow and their contribution to skeletal outcomes during weight loss in obese elderly. Macro- and micronutrient deficiencies are common among elderly individuals, due to altered lifestyle or metabolism. These may be exacerbated by energy-deficient diets, which frequently lack key nutrients for skeletal health including protein, vitamin D, and calcium. This suggests that higher doses of these nutrients or other combined strategies might be needed to mitigate the undesirable weight-loss-induced effects on the skeletal system. The contribution of endocrine factors such as estrogens, insulin-like-growth-factor-1 IGF-1 , leptin, and adiponectin to bone loss observed after weight loss has been detailed elsewhere [ 8 ]. Hereby, we summarize the key findings in older obese individuals. Although reductions in estradiol levels have been reported in obese older women and men during weight loss, possibly due to the reduction of fat mass, these were not correlated with bone loss. Thus, estradiol probably exerts indirect rather than direct effects on bone responses to weight loss [ 37, 42, 56 ]. IGF-1 reductions have been inconsistently reported in older adults under energy or protein restriction [ 37, 42 ]. However, it is unclear whether the absence of changes reflects true effects of the intervention or whether IGF-1 reductions are masked by increases in its binding proteins [ 60 ]. A reduction in leptin, an adipokine significantly involved in the regulation of energy metabolism and with established central and peripheral effects on bone [ 56 ], is a consistent finding among obese elderly weight losers [ 37, 42 ]. In contrast, the role of adiponectin, another adipokine with potential action on bone [ 61 ], in skeletal changes in obese elderly under weight loss remains poorly understood. Inflammation also contributes to sarcopenia by accelerating protein degradation and slowing down protein synthesis in the muscle [ 56 ]. It is widely accepted that aging, obesity, and exercise are characterized by chronic low-grade inflammation, and weight loss reduces inflammatory markers [ ]. However, the effects of weight loss and exercise on inflammatory molecules and processes in relation to skeletal health outcomes in older obese individuals require further elucidation. Besides, a complex interplay exists between bone and inflammatory factors derived from muscle, adipose tissue, brain, the immune system, and host — gut microbiota interactions, which might be further modified by weight loss and exercise during aging [ 66 ]. Animal studies complement and extend research in humans by allowing a detailed examination of caloric restriction, exercise, or nutrient manipulation under standardized conditions and by addressing mechanistic aspects. One of the strengths of animal studies is the existence of similarities in age-related bone loss and obesity among animals and humans. Further advantages of animal studies include the accurate control of diet and exercise, the employment of many study arms, and the ability to analyze changes at different levels [ ]. These advantages are contrasted by a significant diversity among different animal models. The use of animal models requires knowledge of the respective bone anatomy, physiology, energy homeostasis, and the differences between these parameters in animals and humans [ ]. Despite the differences, meticulously designed experimental studies in animals, accompanied by critical data interpretation, have great potential to enhance our knowledge in this area. Surprisingly, we found no previous study on the effects of caloric restriction on skeletal health in obese aged animals, underpinning a significant literature gap in this age group. Current evidence is derived from research in lean aged animals [ 57, ] or obese mature animals [ ], which cannot be extrapolated to obese aged animals. As such, we hereby present available animal models that capture age-related bone loss and obesity. We also propose potentially relevant models, which, however, require validation prior to their use in future weight loss interventions Fig. Advantages and disadvantages of small e. Excellent reviews have described animal models of senile osteoporosis [ 67, 79 ] and obesity [ 68, 80 ]; however, models including both phenotypes are scarce [ 81 ]. A simple and useful model may be the application of a diet-induced obesity DIO paradigm in young, mature, or aged animals. In the DIO paradigm, animals are provided ad libitum access to energy-dense diets, and the progression of obesity and its metabolic consequences are monitored [ 76, 81 ]. Despite its validity and relevance to human obesity, the DIO paradigm is influenced by animal characteristics e. Similarly, aged Sprague-Dawley rats have severe abnormalities in trabecular bone and imbalanced bone turnover favoring bone resorption [ 87 ]. Furthermore, progressive increases in body fat percentage and body fat to lean mass ratio have been reported in Sprague-Dawley rats monitored from the age of 8 to 24 months [ 88 ]. Dietary manipulations and characterization of the body composition of animals with senile osteoporosis may provide new alleys of investigation. The same is true for the determination of skeletal features in established animal models of obesity. For instance, senescence-accelerated mouse-P lines are featured by an accelerated aging phenotype and a short lifespan [ 89 ]. The senescence-accelerated mouse-P6 mice have been established as a model of senile osteoporosis: they exhibit low peak bone mass due to low bone formation and are prone to spontaneous fractures [ 90 ]. Nevertheless, these mice have not been used in diet-induced weight loss interventions. Finally, the use of larger animal models such as dogs, sheep, and pigs might be promising for future research because they offer significant advantages compared to smaller animals [ 79 ]. These include their greater phenotypical similarities to humans and the possibility to collect larger blood volumes over time for biochemical analyses Fig. Nevertheless, their use in age-related research is hampered by their long life span, high costs, handling, housing requirements, and ethical implications. The effects of intentional weight loss in obese older individuals are of clinical significance because this population is susceptible to poor musculoskeletal health even prior to weight reduction. Prospective studies suggest that weight loss is associated with bone loss, impaired bone microstructure, and a higher risk of fractures in elderly. However, these associations often reflect the negative impact of unintentional weight loss in underweight older individuals rather than the effects of intentional weight loss in their obese counterparts. Interventional studies support the worsening of musculoskeletal health outcomes. Nevertheless, these effects appear to be relatively small following a single weight loss attempt and their contribution to the risk of fractures is unknown. The limited body of data from weight maintenance studies is a cause of concern. These show that bone loss persists during this phase. Given the long-term implications of intentional weight loss or repeated weight reduction efforts, strategies to attenuate the harmful effects of weight loss on bone are clinically relevant but remain understudied in this group. The most compelling evidence for such strategies is derived from studies that combined caloric restriction with resistance training. Some older individuals cannot or do not wish to perform exercise training. Thus, future work should be focused on alternative approaches that may counteract, if not prevent, bone loss during active weight loss and weight maintenance. Simultaneously, the assessment of other geriatric outcomes and biochemical markers could provide mechanistic links between weight loss and bone loss. To this end, the use of relevant animal models serves as a unique opportunity to understand the pathophysiology of weight-loss-associated bone alterations, as well as develop and test potential counteracting strategies for obese elderly. All other authors have no conflicts of interest to declare. All authors reviewed and approved the final manuscript. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Gerontology. Advanced Search. Skip Nav Destination Close navigation menu Article navigation. Volume 66, Issue 1. Epidemiological Studies. Interventional Studies. Animal Studies. Statement of Ethics. Disclosure Statement. Funding Sources. Author Contributions. Article Navigation. Review Articles June 28 Is Weight Loss Harmful for Skeletal Health in Obese Older Adults? Subject Area: Geriatrics and Gerontology. Maria Papageorgiou ; Maria Papageorgiou. a Department of Pathophysiology and Allergy Research, Center of Pathophysiology, Infectiology, and Immunology, Medical University of Vienna, Vienna, Austria. b Department of Academic Diabetes, Endocrinology and Metabolism, Hull York Medical School, University of Hull, Hull, United Kingdom. This Site. Google Scholar. Katharina Kerschan-Schindl ; Katharina Kerschan-Schindl. c Department of Physical Medicine, Rehabilitation and Occupational Therapy, Medical University of Vienna, Vienna, Austria. Thozhukat Sathyapalan ; Thozhukat Sathyapalan. Peter Pietschmann Peter Pietschmann. pietschmann meduniwien. Gerontology 66 1 : 2— Article history Received:. Cite Icon Cite. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Table 1. View large. View Large. Table 2. View large Download slide. Proposed mechanisms underlying bone loss during intentional weight loss in obese older adults. is the recipient of a postdoctoral Ernst Mach Fellowship. The authors have no ethical conflicts to disclose. No funding was granted for this work. Prevalence of adult overweight and obesity in 20 European countries, Search ADS. Prevalence of obesity among adults and youth: United States, — NCHS data brief, no Obesity Management Task Force of the European Association for the Study of Obesity. Prevalence, pathophysiology, health consequences and treatment options of obesity in the elderly: a guideline. Osteosarcopenic obesity syndrome: what is it and how can it be identified and diagnosed? Intentional weight loss in older adults: useful or wasting disease generating strategy? Does diet-Induced weight loss lead to bone loss in overweight or obese adults? A systematic review and meta-analysis of clinical trials. Bone loss, physical activity, and weight change in elderly women: the Dubbo Osteoporosis Epidemiology Study. Risk factors for longitudinal bone loss in elderly men and women: the Framingham Osteoporosis Study. Intentional and unintentional weight loss increase bone loss and hip fracture risk in older women. Weight loss: a determinant of hip bone loss in older men and women. The Rancho Bernardo Study. Body weight change since menopause and percentage body fat mass are predictors of subsequent bone mineral density change of the proximal femur in women aged 75 years and older: results of a 5 year prospective study. Risk factors for bone loss in the hip of year-old women: a 4-year follow-up study. The role of fat and lean mass in bone loss in older men: findings from the CHAMP study. Weight change over three decades and the risk of osteoporosis in men: the Norwegian Epidemiological Osteoporosis Studies NOREPOS. Voluntary weight reduction in older men increases hip bone loss: the osteoporotic fractures in men study. What is the influence of weight change on forearm bone mineral density in peri- and postmenopausal women? The health study of Nord-Trondelag, Norway. Predictors of change of trabecular bone score TBS in older men: results from the Osteoporotic Fractures in Men MrOS Study. Long-Term and Recent Weight Change Are Associated With Reduced Peripheral Bone Density, Deficits in Bone Microarchitecture, and Decreased Bone Strength: The Framingham Osteoporosis Study. Osteoporotic Fractures in Men MrOS Research Group. Accelerated bone loss in older men: effects on bone microarchitecture and strength. Weight loss in men in late life and bone strength and microarchitecture: a prospective study. Weight change between age 50 years and old age is associated with risk of hip fracture in white women aged 67 years and older. Weight loss from maximum body weight among middle-aged and older white women and the risk of hip fracture: the NHANES I epidemiologic follow-up study. Weight loss and distal forearm fractures in postmenopausal women: the Nord-Trøndelag health study, Norway. Increase in Fracture Risk Following Unintentional Weight Loss in Postmenopausal Women: The Global Longitudinal Study of Osteoporosis in Women. Risk factors for hip fracture in white men: the NHANES I Epidemiologic Follow-up Study. Weight loss in obese older adults increases serum sclerostin and impairs hip geometry but both are prevented by exercise training. Association between weight cycling history and bone mineral density in premenopausal women. Does recalled dieting increase the risk of non-vertebral osteoporotic fractures? The Tromsø Study. Weight cycling and risk of forearm fractures: a year follow-up of men in the Oslo Study. Weight loss, exercise, or both and physical function in obese older adults. Exercise training in obese older adults prevents increase in bone turnover and attenuates decrease in hip bone mineral density induced by weight loss despite decline in bone-active hormones. Weighted vest use during dietary weight loss on bone health in older adults with obesity. Effect of exercise modality during weight loss on bone health in older adults with obesity and cardiovascular disease or metabolic syndrome: a randomized controlled trial. Effect of voluntary weight loss on bone mineral density in older overweight women. Very low calorie diets for weight loss in obese older adults-a randomized trial. Effect of weight loss and exercise therapy on bone metabolism and mass in obese older adults: a one-year randomized controlled trial. Does high-intensity resistance training maintain bone mass during moderate weight loss in older overweight adults with type 2 diabetes? Armamento-Villareal R1, Qualls C. Aerobic or resistance exercise, or both, in dieting obese older adults. Change in bone mineral density during weight loss with resistance versus aerobic exercise training in older adults. Prediction of lumbar vertebral body compressive strength of overweight and obese older adults using morphed subject-specific finite-element models to evaluate the effects of weight loss. Long-term maintenance of weight loss after lifestyle intervention in frail, obese older adults. Weight loss interventions in older adults with obesity: a systematic review of randomized controlled trials since Why the ISMNI and the Utah paradigm? Their role in skeletal and extraskeletal disorders. As you can see, osteoporosis undermines bone strength and resilience not only by decreasing bone mass total tissue but also by disrupting the bone's "microarchitecture," or structural organization. Another 22 million women are at increased risk for the disease. In both sexes, certain medications glucocorticoids, aromatase inhibitors, immunosuppressive drugs, chemotherapy drugs, and anticonvulsants can lead to significant bone loss. So can certain medical conditions. Celiac disease and Crohn's disease, for example, reduce the absorption of calcium and other nutrients needed for bone maintenance. Rheumatoid arthritis, hyperthyroidism, chronic kidney or liver disease, osteogenesis imperfecta, and anorexia nervosa are also associated with osteoporosis. Currently, a woman's odds of having an osteoporotic fracture are one in three. We can't control all the factors involved, but we need to do all we can to strengthen and preserve our bones. To that end, here are eight important points to keep in mind. A healthy diet preserves bone strength by providing key nutrients such as potassium, magnesium, phosphorus, and — of course — calcium and vitamin D. If you don't get enough calcium, your body will take it from your bones. If your diet doesn't supply enough calcium 1, to 1, milligrams per day , take a supplement. The same goes for vitamin D, which is needed to extract calcium from your food. Food sources of vitamin D are limited, and you may not get enough sun to manufacture adequate amounts through the skin. Experts recommend to 1, IU of vitamin D per day women being treated for vitamin D deficiency take much higher amounts. According to the National Osteoporosis Foundation, vitamin D 3 cholecalciferol is the form that best supports bone health. To learn more about other nutrients that affect bone health, visit www. Two types of exercise — weight-bearing and resistance — are particularly important for countering osteoporosis. Weight-bearing activities are those in which your feet and legs bear your full weight. This puts stress on the bones of your lower body and spine, stimulating bone cell activity. Weight-bearing exercise includes running, jogging, brisk walking, jumping, playing tennis, and stair climbing. Resistance exercise — using free weights, rubber stretch bands, or the weight of your own body as in sit-ups and push-ups — applies stress to bones by way of the muscles. It's especially helpful for strengthening bones of the upper body that don't bear much weight during everyday activities. Merely occasional exercise won't help, though. Aim for at least 30 minutes of bone-strengthening exercise most days of the week. If you have osteoporosis or another pre-existing health condition, consult a clinician about whether you should avoid certain activities, positions, or movements. Bone continually undergoes a process called remodeling, or bone turnover, which has two distinct stages: resorption breakdown and formation. Bone is a storage depot for calcium. When the body needs calcium, bone cells called osteoclasts attach to the bone surface and break it down, leaving small cavities A. Bone-forming cells called osteoblasts move into these cavities B , releasing collagen and other proteins to stimulate bone mineralization and replace what was lost. The osteoblasts that become incorporated in the new bone matrix are called osteocytes C. Early in life, bone formation outpaces resorption. By age 20, most of us have the greatest amount of bone tissue we'll ever have peak bone mass. Bone mass declines very slowly until late perimenopause, when bone loss becomes more rapid, due in part to decreased estrogen, a crucial player in bone turnover. Also, after age 50 to 60 our bodies are less able to absorb calcium and produce vitamin D. We continue to lose bone, though more slowly, for the rest of our lives. Here's yet one more reason not to smoke: Women who smoke lose bone faster, reach menopause two years earlier, and have higher postmenopausal fracture rates. The mechanism isn't known; smoking may lower estrogen levels, or it may interfere with the absorption of calcium and other important nutrients. To screen for osteoporosis, clinicians measure bone mineral density BMD — the amount of calcium and other minerals in bone. The best way to assess fracture risk is to calculate BMD at the spine and hip with low-dose x-rays dual-energy x-ray absorptiometry, or DXA and factor in a woman's age. The World Health Organization's definition of osteoporosis is based on a DXA value called a T-score, which compares the amount of bone a woman has to normal peak bone mass. Most official guidelines recommend DXA screening for all women starting at age 65, and earlier for women who take medications or have health conditions that increase osteoporosis risk. But reduced BMD is only one risk factor for osteoporosis. You're also at greater risk if you smoke or are older, Caucasian, or thin, or if you had a fracture after age 50 or have a parent who had a hip fracture. The World Health Organization has developed a formula that predicts year fracture risk based on BMD and other risk factors. A calculator based on this formula is available at courses. Clinicians are also interested in bone quality — a complex characteristic that includes bone mineralization, microarchitecture, and the rate of bone turnover. So far, we have no way to noninvasively assess bone quality, but new imaging technologies are being developed that may allow clinicians to visualize the internal structure of bone and gain information that was once available only through biopsy. Most approved osteoporosis drugs see sidebar are antiresorptive, that is, they slow resorption, the breakdown phase of bone turnover. Only one drug, parathyroid hormone Forteo , is anabolic, meaning that it stimulates new bone formation. All medications have side effects, and dosing schedules vary from one to the other, so it's important to explore all the options with your clinician. One adverse effect of bisphosphonates — death of jawbone tissue, usually after dental extractions or oral surgery — has occurred extremely rarely in women taking bisphosphonates for osteoporosis. It mostly has affected cancer patients, who take far higher bisphosphonate doses, usually intravenously. Several osteoporosis drugs are under investigation, including the mineral strontium in the form of strontium ranelate, and denosumab, a monoclonal antibody that works by blocking osteoclasts, the cells that resorb bone. No longer a first-line therapy. Since the mids, researchers have investigated links between depression and bone loss. In , a New England Journal of Medicine study found that women with a history of major depression had lower bone density at the hip and spine and higher levels of cortisol, a stress hormone associated with bone loss. Since then, many studies have found a similar relationship. Research has also linked selective serotonin reuptake inhibitor antidepressants with fractures, but cause and effect has not been established. It may be a long time before these connections are fully elucidated. In the meantime, women being treated for depression may want to talk to their clinicians about a BMD test. Weighing less than pounds or having a body mass index under 21 is a risk factor for osteoporosis. Regardless of your body mass index, if you lose weight during the menopausal transition late perimenopause and the first few years after menopause , you're more likely to lose bone. Avoid ultra-low-calorie diets and diets that eliminate whole food groups. |
Wacker, dieser Gedanke fällt gerade übrigens